Damiano Rondelli
Chicago, Illinois, United States
 |
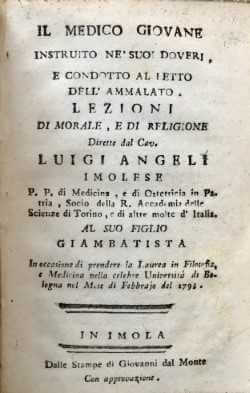
In a rare text from 1793, the Italian physician Luigi Angeli instructed young doctors on how to approach a patient: “. . . once you questioned the patient about his disease, or the remote causes of this, and after you observed the quality of his temper, age, once clarified the life style, occupations, or any other personal circumstance, you will show soon your personal interest for him and slowly will make him understand your love. This familiarity will allow you to understand the patient’s fears, weaknesses and even the quirks . . .”1
More than two hundred years later the medical community acknowledges the ethical value of this approach, but also faces pressures to be efficient. It is often heard that patient flow needs to increase to make hospital practice sustainable [i.e. profitable], pay the bills, and support the growth of the institution. If someone says: “I really need to spend time with my patients to make sure that everything is covered,” that intention is welcomed. But if it means: “Therefore, I can only see five patients today,” the budget may not cover that doctor’s salary.
Time is not the only variable needed to provide good care, since the doctor should identify the one or few health problems among many that need to be prioritized. But let us assume that everyone is a good clinician and has many patients. When we go to the clinic and look at the list of twenty-five patients scheduled in the morning, we experience an immediate sense of disciplined timing. The patient is often the target of a professionally crafted sequence of standardized questions and physical examination maneuvers that allow the doctor to efficiently go over past medical history, clinical assessment, test results, medication list, a brief lecture on current disease status and plans, and a handshake with the time for the next appointment.
Sometimes we “attack” our patients with a long list of words intended to be simple and clear and address the patient’s questions even before they are asked. At the end of an overwhelming and rapid monologue, we ask: “Are there any questions?” Many patients feel they would annoy the doctor by asking questions, or would look dumb by admitting that our explanation was not clear, so they just say “thank you” and the visit is over on time! However, some patients will challenge us with questions, indicate that we were not very clear, and request extra explanations. This makes us nervous because the clock is ticking and we need to cut short the next patient to catch up on time.
Many patients say they feel nervous for a few days before coming to the clinic. They do not sleep well, and are anxious to know if their cancer is in remission, or has recurred, or if their labs have improved since the last visit. As I enter the room their eyes speak louder than their words, and they are ready to read and interpret my body language before hearing what I have to say. A smile will reassure them, a deep breath and a slow initial introduction will sound like trouble. I imagine the day of the visit has been highlighted in the patient’s calendar for weeks. But on the doctor’s list of the day, that visit is only a number to go through before going home or on to the next endeavor.
The decision to become a doctor is made for very personal reasons, but the decision one makes to take care of patients is sometimes forgotten, or lost through life changes, or neglected for different reasons. My own career and responsibilities have changed over the years, and my original motivation has been shaped by an academic environment providing scenarios that go beyond individual patient care. However, my perspective on patients has not changed. I feel privileged to be reminded daily of the value and dignity of every human being. We all need to be reminded of the absolute value of those we serve and maintain a human approach independent of time, money, opinions, and environment.
When I make morning rounds and have twenty rooms to enter with residents and fellows, I am aware that the five or ten minutes spent with the patient is:
- the most important thing he has been waiting for that day;
- what she will immediately report to the family visiting in the hospital, or by phone, as soon as I leave the room;
- gives the patient a feeling of being taken care of and that there is a plan to look forward to;
- an opportunity for me to share with younger doctors the value of a human connection with the patient.
The time spent with a patient is about that person, not just my clinical plan. It requires a focus on clinical issues, diagnostic hints, and questions that can reveal unspoken symptoms or obstacles to care such as family, transportation, or financial circumstances. It is important to listen to the patient’s own description of what is going on in addition to my assessment. My clinical assessment might describe “mild mucositis post chemotherapy, based on mild erythema of the buccal mucosa and difficulty in having solid food.” The patient’s own description may be: “Doctor, it hurts like hell when I try to eat solid food and I am stuck with soups!”
 |
Maintaining a patient focus allows us to capture a context where clinical, social, and personal elements help us formulate the best treatment strategy and appropriate and personalized recommendations to best achieve a patient’s compliance and consistence. Communication is not only about “covering the bases” to make sure that I mentioned every possible risk or side effect (without verification that the patient really understood), but is also showing empathy, and demonstrating I really believe that what I am recommending is the best option for the patient, as Dr. Angeli recommended in 1793.
When I stand by a hospital bed, I tell my patient on chemotherapy that we are on the same side and will journey together through good and bad days. Sometimes that means sharing moments of personal life, such as family events, stories of children, travel plans or, in my case, Italian food suggestions. It takes only a few minutes to enter into their world, and they will remember this. Three months later they will ask of my trip to Italy, or let me know of their daughter’s wedding. Sharing patient journeys have presented amazing and unique opportunities over the years, such as playing the guitar with a mariachi band, or riding horses together. At times, however, it has also meant facing treatment failure, hopelessness, the anticipation of “nothing else to do,” and moments of silence with nothing more to say that, “We have done everything we could. We face a disease stronger than our treatment.” It is humbling and touching when what I receive from a patient or family in those moments is, “Thank you, Doctor. We really appreciate everything you have done.” Sometimes indeed I have walked out of a room with tears in my eyes.
At the end of one clinic day, though feeling tired, I often recall all the patients I saw and remember their faces, diagnoses, difficult choices, unknown outcomes, and family problems. I have other days filled with people meeting with me for different reasons, from administrative purposes to clinical decisions; research plans to personal issues. There are so many meetings, people, and responsibilities that must be dealt with on a daily basis. We expect that our actions will result in both healing and efficiency, but we are challenged by obstacles thrown at us by unpredictable circumstances. How many times do we end our day with: “I did not do even half of the things I had planned today,” or “I am exhausted and do not even remember what I did the whole day,” or “It took me the whole morning to deal with what I thought would take me fifteen minutes”?
The book From Values to Action2 has made me think about what I do every day. Author Harry Kraemer suggests that you can do a hundred things and each will be successful, but you will move from success to significance only if these things have a connection with who you are and to what is relevant in your life. A passion for the dignity of any patient can be a five- or fifty-minute business, but it always has the same root, which is the connection between that person and the meaning of your whole life. Kraemer also explains that in order to move from success to significance we need to take some time to think about the significance of what we would like to bring to our activities before we start doing them.
I hope to bring with me to every patient encounter a desire to help and a passion to serve those in need, as well as professional skill, courage, and enthusiasm. In the clinic there are time constraints, delays, and sometimes patients are overbooked, but the desire to make them better is an overriding recipe for efficiency and also for healing. In my early career I was inspired by older doctors. It is now my hope to inspire others to see the same beauty.
A young fellow who had trained with us in hematology/oncology almost eight years ago asked me to go with him to his country where he wanted to support medical education. This is how I started going to Kathmandu in Nepal. That passion rapidly became a project to help poor countries build capacity to take care of patients with blood diseases in need of a bone marrow transplant. After six years of close collaboration, Nepal has now a state-of-the-art Bone Marrow Transplant program in a public hospital where a transplant costs $4,000, as opposed to $200,000 or more in the United States.
My conclusion is that healing and efficiency are not incompatible. They can be achieved once we begin seeing patients as people and not as numbers.
References
- Angeli L. Il medico giovane instruito ne’ suoi doveri, e condotto al letto dell’ammalato. IMOLA, Stamperia Giovanni dal Monte, 1793
- Kraemer HM. From Values to Action: The Four Principles of Value-Based Leadership. Jossey-Bass, 2011
DAMIANO RONDELLI, MD, is the Michael Reese Professor of Hematology, Chief of the Division of Hematology/Oncology, and Director of the Blood and Marrow Transplant at the University of Illinois Hospital & Health Sciences System in Chicago, Illinois.
Spring 2018 | Sections | Doctors, Patients, & Diseases

Leave a Reply