Sue Reeves
Roehampton, London, UK
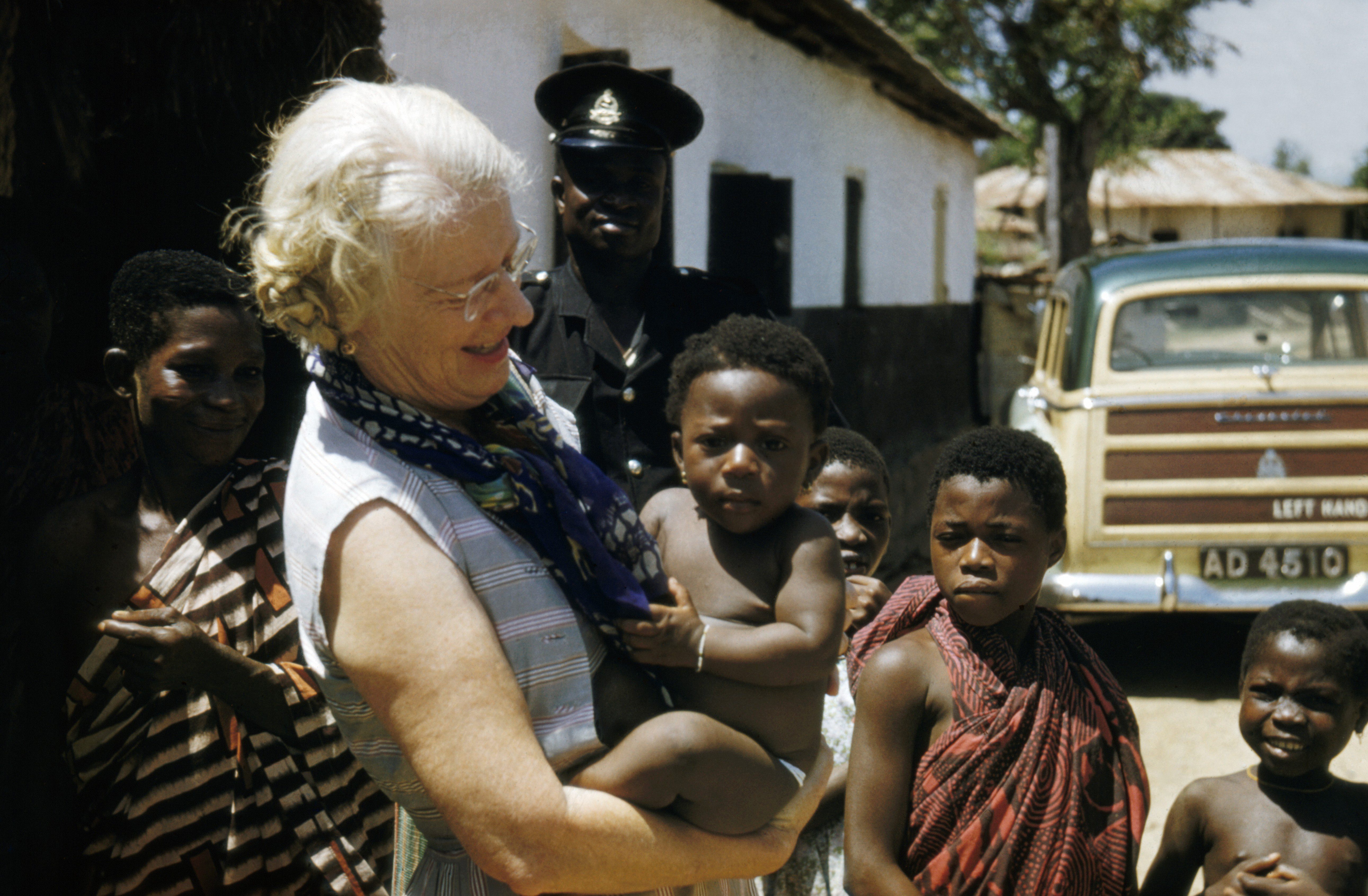 |
| Figure 1. Dr Cicely Williams in later years on a visit to Ghana (The Wellcome Trust, London). |
Cicely Delphine Williams (1893-1992) has been described as achieving the ‘physician’s dream’1 by diagnosing, identifying the cause, and finding a prevention and a cure for a disease.2 The disease she identified was kwashiorkor, a severe form of protein-energy malnutrition, fatal if not treated promptly. Williams was the first woman to recognize and conduct research on kwashiorkor and differentiate it from other dietary deficiencies.
Jamaican born Williams’ medical career began in 1916 when she became one of the first women to study medicine at Somerville College, University of Oxford.3 After completing her medical training at Kings College Hospital she undertook a further course in tropical medicine before travelling to the west coast of Africa as a woman medical officer.4 She first came across kwashiorkor while working in Accra on the Gold Coast, known today as Ghana. The symptoms of kwashiorkor to quote Williams are: “oedema chiefly of the hands and feet, followed by wasting, diarrhoea, irritability, sores and desquamation of areas of the skin.”5 Her description of the symptoms of kwashiorkor is still used in text books today.6 Williams remarked, “It appears to be due to some dietetic deficiency.”5 The disease was seen when breast feeding had been reduced and supplementary weaning food consisted largely of maize. White maize was frequently eaten, partially fermented to make a gruel known as arkasa or sometimes as a thicker dough called kenki.7 Williams pointed out when “maize was the only source of the supplementary food, some amino acid or protein deficiency cannot be excluded as a cause.”5 The word ‘kwashiorkor’ could be described as a polyseme since it not only represents the biomedical symptoms, but also reflects the social situation since the word comes from the Ga Language and means ‘disease of the deposed child’ and is a reflection of the sibling birth position.8
Williams published her first paper on kwashiorkor in the Archives of Disease in Childhood in 19335. The term kwashiorkor was not used, rather this paper described a nutritional disease of childhood associated with a maize diet. However not everyone accepted Williams’ interpretation of the disease, and many consultants believed she simply didn’t recognise the symptoms of pellagra (vitamin B3 deficiency). Not least Dr Hugh Stannus who also published a paper in the Archives of Disease of Childhood in 1934 where he “disputed the correctness of the diagnosis” and suggested Williams simply did not recognise pellagra.9 As a rebuttal Williams wrote a paper published in the Lancet with ‘kwashiorkor’ blatantly in the title 7 and included a table marking notable differences between pellagra and kwashiorkor. She wrote that in her experience kwashiorkor usually occurred in children under the age of five years yet was not seen in adults, whereas pellagra was more common in adults.
It took over twenty years for kwashiorkor to be recognised and accepted by the medical establishment, 2 but Williams’ explanation of kwashiorkor is still valid and used today.6 Research is being done on the role of other micronutrients, though sadly there is still a high fatality rate in some parts of the world.10
Williams’ story, however, does not end there. After working on the Gold Coast for many years, she was transferred to Malaya where she continued her work with mothers and children. During the World War II Japanese invasion in 1941, she made a ten day trek from Malaya through the jungle to Singapore, and in the bottom of her rucksack she carried the notes she had made on a different dietary deficiency, this time rickets.11 Before long the Japanese arrived in Singapore, and she was sent to Changi prison for a period of three years, where she was accused of being spy3 and was forced to endure horrendous conditions and suffering.12 Williams’ notes on rickets even went with her into internment at Changi which, in her paper published in 1946 she writes, “afforded leisure to write them up”.11 She also offered apologies for defects in the paper because she had no access to hospital records and books. After the war Williams returned to Malaya to organise the rural health service before she was made the first director of Maternal and Child Welfare for the World Health Organisation in Geneva. Always preferring to practice medicine rather than being desk-bound,13 she worked in many countries in Africa and the Middle East before retiring in Oxford, England.
Williams will always be remembered for her vital and ground breaking work with mothers and children around the world, and her name will be forever be synonymous with the discovery and treatment of kwashiorkor. She thus achieved the physician’s dream.
References
- Williams CD, Baumslag N, World Federation of Public Health Associations & UNICEF (1986) Primary health care pioneer: The selected works of Dr. Cicely D. Williams. Geneva, Switzerland: World Federation of Public Health Associations and UNICEF.
- Stanton J (2001) Listening to the Ga: Cicely Williams’ Discovery of Kwashiorkor on the Gold Coast. Clio Medica, 61, 149-171.
- Somerville College Archives http://blogs.some.ox.ac.uk/archive/ Accessed 8.3.16
- Stanton J (1992) Obituary: Dr Cicely Williams. Independent, Wednesday 15 July 1992.
- Williams C (1933) A nutritional disease of children associated with a maize diet Arch Dis Child, 8, 423-428.
- Mann J & Truswell AS (2002) Essentials of Human Nutrition 2nd edition Oxford: OUP
- Williams CD (1935) Kwashiorkor: a nutritional disease of children associated with a maize diet.Lancet, 229, 1151-1152.
- Konotey-Ahulu FID (2005) There is nothing mysterious about kwashiorkor. Brit Med J, 330, 1095.
- Stannus HS (1934) A nutritional disease of childhood associated with a maize diet – and pellagra. Arch Dis Child, 9, 50, 115-118.
- Krawinkel M (2003) Kwashiorkor is still not fully understood Bull World Health Org 81 http://dx.doi.org/10.1590/S0042-96862003001200010
- Williams CD (1946) Rickets in Singapore. Arch Dis Child, 21, 105, 37-51.
- Craddock S (1983) Retired except on Demand: the life of Dr Cicely Williams. Oxford: Green College
- Gairdiner D (1984) Book review. Arch Dis Child, 59, 392-394.
DR. SUE REEVES, RNutr, is a Principal Lecturer, registered nutritionist, researcher and convener of the Nutrition and Health program at the University of Roehampton, London. Part of this work was conducted while as a visiting scholar at St John’s College, University of Oxford.
Spring 2016 | Sections | Women in Medicine

Leave a Reply